Managing FAIS Without Surgery: The Role of Rehabilitation in Hip Pain
Hip pain and mobility issues can be frustrating for both patients and clinicians, especially when FAIS is diagnosed. Learn why conservative care should come first, with strategies to restore function and avoid surgery.
March 4, 2025
10 min. read

Femoroacetabular impingement syndrome (FAIS) has become an increasingly recognized cause of hip and groin pain, particularly in young, active individuals. Historically, its treatment has centered on hip arthroscopy, a surgical procedure aimed at correcting bony abnormalities believed to contribute to impingement.
Emerging evidence indicates that structural changes alone do not dictate symptoms, leading to a shift toward conservative management strategies, including physical therapy, manual therapy, and exercise-based rehabilitation.
Understanding the evolving landscape of FAIS management is critical for clinicians. As more patients are diagnosed with FAIS, many are rushed into surgery before conservative options are fully explored. But is surgery always necessary?
In this article, we will evaluate why a conservative approach should be the first line of treatment, the biomechanical factors contributing to FAIS, and how clinicians can optimize rehabilitation strategies to help patients avoid unnecessary surgery.
Rethinking the cause of FAIS: More than just bone structure
For years, cam and pincer morphologies—bony changes at the femoral head-neck junction and acetabulum—were considered the primary culprits in femoroacetabular impingement syndrome. Recent research challenges this idea, showing that structural abnormalities alone do not dictate symptoms.
Bony abnormalities do not always cause symptoms. Many individuals with FAIS-related changes on imaging are completely asymptomatic.1
Microinstability and soft tissue dysfunction contribute significantly to pain and movement impairment. Weakness in the deep hip stabilizers, repetitive mechanical loading, and muscle imbalances disrupt joint mechanics, leading to excessive translation and altered movement patterns.2,3
FAIS is more than just an “impingement problem”—it's a movement disorder requiring a neuromuscular approach to rehabilitation. Repetitive anterior hip joint loading, compensatory muscle patterns, and joint microinstability play a larger role in symptom development than previously thought.4
These findings align with other paradigm shifts in orthopedic care. In shoulder rehabilitation, subacromial decompression surgery was once considered the gold standard for impingement. However, exercise therapy has since proven just as effective—if not superior—for many patients.
The same may hold true for hip impingement. While bony changes like cam and pincer deformities were historically blamed for FAIS symptoms, we now recognize that muscle imbalances, soft tissue dysfunction, and movement impairments play a more significant role in pain development.
Why physical therapy should be the first line of treatment
For many patients diagnosed with FAIS, the first instinct is to seek surgical correction. After all, if imaging shows a bony abnormality, wouldn’t removing it fix the problem? But pain and dysfunction often stem from movement impairments, muscle imbalances, and joint instability—not just bone structure. Before considering surgery, clinicians should first determine whether targeted rehabilitation can restore function and relieve pain—often with outcomes comparable to surgery. Here’s why a conservative approach should be the first line of treatment:
Surgery doesn't address the underlying problem
Hip arthroscopy can reshape bone and repair labral tears, but it does not correct the faulty movement patterns driving pain and dysfunction. While surgery may improve symptoms for some, revision hip arthroscopy is required in 5 to 14 percent of patients following the initial procedure, and outcomes remain variable.5
Removing excess bone may temporarily reduce impingement, but it does not resolve dysfunctional movement patterns, increasing the likelihood of symptom recurrence. Without addressing these underlying deficits, patients remain at risk for continued pain, movement impairments, and the need for additional interventions.
Exercise-based rehabilitation can be highly effective
Emerging research suggests that well-designed conservative programs can produce outcomes comparable to surgery. Physical therapy interventions for patients with FAIS should focus on the following:
Improving posterior chain activation: Weakness in the gluteals and deep hip stabilizers often leads to compensatory overuse of the hip flexors and anterior structures. To restore balance and optimize movement mechanics, exercises targeting the gluteus medius, deep external rotators, and hamstrings—such as lateral band walks, Romanian deadlifts, and sidelying hip abduction—are essential.
Addressing movement patterns: Patients often demonstrate excessive hip adduction and internal rotation during functional activities. Neuromuscular retraining, including gait modifications, postural education, and movement re-patterning, can help redistribute joint loading.
Enhancing mobility while maintaining joint stability: Manual therapy techniques, including anterior hip mobilizations, soft tissue work for the iliopsoas, and posterior capsule mobilizations, can improve hip mechanics and reduce anterior joint compression.
How to build an effective conservative treatment plan
While surgery aims to reshape bone, rehabilitation focuses on restoring function, where real, long-term success can happen. A well-structured conservative program doesn’t just relieve pain; it also retrains movement, restores strength, and prevents future injury.
Here’s how you can build a treatment plan that addresses the root causes of FAIS and helps your patients return to peak performance:
1. Reduce pain and restore mobility
At this stage, your goal is to reduce discomfort and restore movement without aggravating symptoms. You can achieve this by:
Teaching patients how to modify aggravating activities, such as avoiding prolonged sitting or deep squatting.
Utilizing soft tissue work, joint mobilizations, and activity modification to alleviate symptoms.
Incorporating isometric exercises to activate and strengthen the deep hip stabilizers without excessive joint strain.
2. Improve neuromuscular control and strength
At this point, your focus shifts from pain relief to restoring strength and movement efficiency. Traditional rehabilitation for FAIS has often relied on uniplanar, non-weight-bearing exercises, which fail to prepare patients for the dynamic, multiplanar nature of real-world movement. Since FAIS is driven by triplanar, weight-bearing demands, rehabilitation must reflect these complexities.
To help your patients regain stability and prevent compensatory patterns, you should:
Strengthen the posterior chain by targeting the glutes, hamstrings, and hip abductors to improve hip stability.
Retrain movement patterns to correct faulty mechanics and reduce excessive hip adduction and internal rotation.
Progressively load the hip joint through controlled resistance exercises to enhance strength and endurance.
3. Return to high-level function and sport-specific movements
In this final phase, your focus is on preparing your patients for the demands of daily life, work, or sport. Since FAIS is driven by triplanar, weight-bearing movements, rehabilitation at this stage should reflect the complexity of real-world activities. To ensure a successful return to activity and long-term resilience, you should:
Incorporate dynamic stability drills and reactive control training to help your patients develop better movement control under load and in unpredictable situations.
Implement sport-specific training that mimics the movements and forces required for their activities, ensuring a safe and effective transition back to performance.
Develop long-term maintenance strategies by educating your patients on self-management techniques, progressive loading, and ongoing strength and mobility work to prevent symptom recurrence.
By integrating triplanar, weight-bearing movements and progressively challenging neuromuscular control, our treatment approach better reflects the demands placed upon the body—leading to more effective, lasting outcomes.
Rehabilitation over surgery: A patient success story
Emma, a 26-year-old competitive soccer player, began experiencing deep anterior hip pain that worsened with sprinting, cutting, and prolonged sitting. Concerned about her ability to continue playing, she sought medical advice and was diagnosed with femoroacetabular impingement syndrome based on imaging that showed a cam morphology and labral irritation.
An orthopedic surgeon recommended hip arthroscopy to reshape the femoral head and repair the labrum, emphasizing that surgery was the best option for long-term relief, but Emma was hesitant. She wanted to explore conservative treatment first before committing to an invasive procedure.
A structured rehabilitation approach
Emma was referred to a physical therapist who developed a comprehensive rehabilitation plan focused on restoring function, optimizing movement, and addressing the underlying contributors to her pain. Her treatment plan emphasized:
Activity modification and load management: Identifying and adjusting movement patterns that placed excessive stress on her hip joint. Emma was advised to limit deep hip flexion and excessive internal rotation to reduce mechanical strain.
Neuromuscular re-education: Addressing weakness in the deep hip stabilizers and inefficient movement patterns through gait retraining and targeted strengthening to improve joint mechanics and movement efficiency.
Progressive strengthening and mobility work: Implementing a three-phase rehab program focused on building strength, improving stability, and gradually restoring hip mobility, ensuring a controlled return to activity without compensation.
Return-to-play progression: Introducing sport-specific movement patterns in a controlled manner, incorporating cutting, sprinting, and lateral movements while reinforcing optimal hip mechanics.
Outcome: Surgery avoided, performance restored
After 16 weeks of progressive rehabilitation, Emma reported significant pain reduction and was able to return to full soccer activities without limitations. Follow-up imaging showed no worsening of her labral irritation, and two years later, she remains symptom-free—without surgery.
Emma’s case highlights a key takeaway: Structural abnormalities alone do not determine the need for surgery. A well-structured rehabilitation program can often help patients manage FAIS conservatively, restore function, and return to high-level activity.
Leading the shift toward evidence-based FAIS management
The rising number of hip arthroscopies highlights a critical question: Are we too quick to operate? While surgery has its place, research continues to support rehabilitation as an effective first-line treatment for many individuals with FAIS. By focusing on movement quality, neuromuscular control, and functional strength, clinicians can help patients not only manage symptoms but return to an active lifestyle—without unnecessary surgery.
Want to stay ahead of the latest evidence and refine your approach to FAIS? Check out my Medbridge courses on femoroacetabular impingement syndrome to deepen your understanding of FAIS epidemiology, risk factors, and structural adaptations while improving clinical diagnosis with the latest evidence. Plus, with hip arthroscopy rates on the rise, learn when surgery is warranted, when conservative care is just as effective, and how to develop an evidence-informed rehab plan.
Femoroacetabular Impingement Syndrome: Background, Diagnosis, Risk Factors
Femoroacetabular Impingement Syndrome: Surgical or Conservative Treatment
References
Griffin, D. R., Dickenson, E. J., O'Donnell, J., Agricola, R., Awan, T., Beck, M., Clohisy, J. C., Dijkstra, H. P., Falvey, E., Gimpel, M., Hinman, R. S., Hölmich, P., Kassarjian, A., Martin, H. D., Martin, R., Mather, R. C., Philippon, M. J., Reiman, M. P., Takla, A., Thorborg, K., … Bennell, K. L. (2016). The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. British journal of sports medicine, 50(19), 1169–1176. https://doi.org/10.1136/bjsports-2016-096743
Casartelli, N. C., Maffiuletti, N. A., Item-Glatthorn, J. F., Staehli, S., Bizzini, M., Impellizzeri, F. M., & Leunig, M. (2011). Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis and cartilage, 19(7), 816–821. https://doi.org/10.1016/j.joca.2011.04.001
Dischiavi, S. L., Wright, A. A., Hegedus, E. J., & Bleakley, C. M. (2019). Rethinking Dynamic Knee Valgus and Its Relation to Knee Injury: Normal Movement Requiring Control, Not Avoidance. The Journal of orthopaedic and sports physical therapy, 49(4), 216–218. https://doi.org/10.2519/jospt.2019.0606
Franklyn-Miller, A., Richter, C., King, E., Gore, S., Moran, K., Strike, S., & Falvey, E. C. (2017). Athletic groin pain (part 2): a prospective cohort study on the biomechanical evaluation of change of direction identifies three clusters of movement patterns. British journal of sports medicine, 51(5), 460–468. https://doi.org/10.1136/bjsports-2016-096050
O'Connor, M., Steinl, G. K., Padaki, A. S., Duchman, K. R., Westermann, R. W., & Lynch, T. S. (2020). Outcomes of Revision Hip Arthroscopic Surgery: A Systematic Review and Meta-analysis. The American journal of sports medicine, 48(5), 1254–1262. https://doi.org/10.1177/0363546519869671
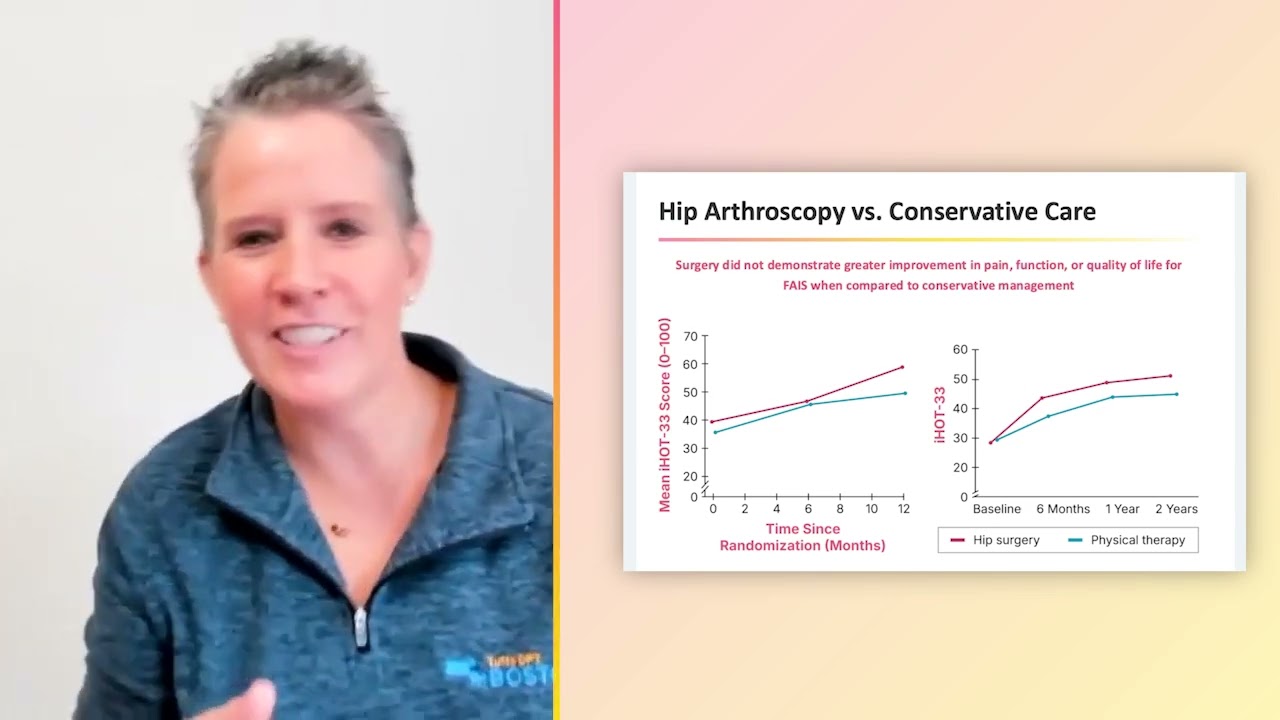
Below, watch Alexis Wright discuss hip arthroscopy vs. conservative care in this brief clip from her Medbridge course "Femoroacetabular Impingement Syndrome: Surgical or Conservative Treatment."